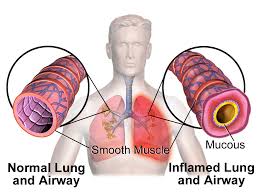
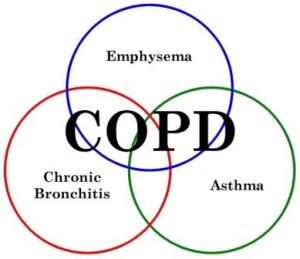
For those that suffer with chronic conditions such as COPD one of the major symptoms that patients suffer with is fatigue and it is important to try and combat this as mobility and exercise is crucial to help curb the disease and its symptoms. Oxygen therapy has been shown to help combat fatigue as the additional oxygen getting into your blood stream will help to supply more oxygen to your cells to help them to function more efficiently and your brain and body in general will feel more alert and active. However if oxygen therapy does not combat your fatigue then eating carnitine-enriched foods or by taking carnitine supplements, could help to combat this.
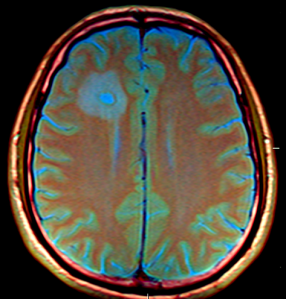
Our bodies produce carnitine naturally in most of our cells from amino acids and it plays a crucial role in energy production within the mitochondria of our cells. It is thought that faulty mitochondria play a vital role in diseases such as COPD and that this may be the cause of the fatigue experienced by patients with chronic conditions as the mitochondria cannot perform its duties and one of these is to produce energy for the cell.
Carnitine transports fatty acids to the mitochondria so they can use it to produce energy and also helps to transport waste products out of the mitochondria to prevent buildup.
A lack of carnitine in our body could be due to a genetic problem or due to metabolic disturbances caused by disease but normally it is produced in sufficient amounts in the liver and kidneys. It has other properties such as being an antioxidant and fights off free radicals, which can damage the cells.
Supplements can be taken or there are foods that contain high levels of carnitine such as beef steak and other red meats, milk, chicken breast and cheddar cheese.
A recent study looking at the effect of taking carnitine when suffering from conditions such as COPD found that ‘these supplements can reduce significantly the fatigue and other symptoms associated with chronic disease and can naturally restore mitochondrial function, even in long-term patients with intractable fatigue.” Other studies have also shown that carnitine supplementation can help with blood supply problems, heart defects and attacks and Alzeihmer’s. Even athletes use carnitine supplementation to help improve performance and reduce muscle fatigue.
References: http://www.medicalnewstoday.com